Many researchers seeking treatments for humanity’s most debilitating conditions – from Alzheimer’s and blindness to heart disease and diabetes – see potential for bettering lives in the foundation of life itself: the cell.
University of Nebraska-Lincoln engineers recently introduced a prototype system that could reduce the cost and complexity of growing patient-derived cells, advancing the cause of personalized therapies that replace damaged or dead cells to regenerate tissues in the body.
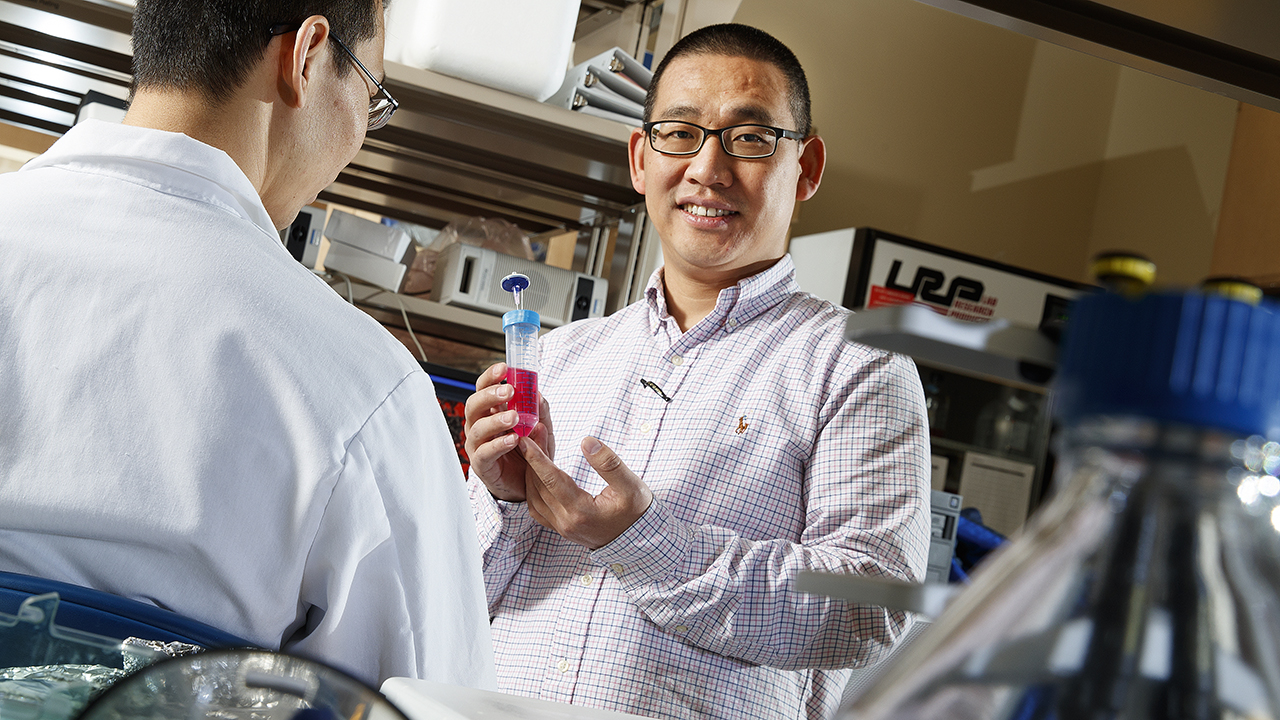
Researcher Yuguo “Leo” Lei designed the system to cultivate induced pluripotent stem cells: adult cells genetically reprogrammed into blank-slate versions that can, in turn, become any of the roughly 200 specialized types in the human body. These stem cells can also replicate again and again outside of the body – important when considering that a regenerative treatment typically requires hundreds of millions or even billions of cells.
Consisting of little more than two hotdog-sized plastic tubes, syringes and an automated pump, Lei’s system cultivates the cells in a substance known as hydrogel. The prototype incorporates three phases of stem-cell processing – replicating them, converting them to specialized cells, and removing unwanted components – into one system, a feat that Lei said could streamline many logistical challenges.
“The idea, in the future, will be to integrate all of this in the clinic,” said Lei, assistant professor of chemical and biomolecular engineering. “You get cells from the patient, and then after processing in a single tube over one or two months, you give the cells back to the patient. That’s the long-term goal.”
By limiting exposure to air, the system lessens the risk of contamination. And though the team demonstrated some of the processing steps by hand, Lei said the prototype lends itself to automation, which would reduce human error and ensure compliance with regulatory protocols. It would also allow the system to operate 24/7, accelerating the production of cells while making cell-based therapies more affordable.
“The majority of the cost is in the labor,” Lei said. “It’s very expensive. This would dramatically reduce that cost.”
Personalized therapies that grow new cells from a patient’s own stock hold promise for treatment because they minimize the risk that the body will perceive and attack them as foreign agents. But growing enough cells for thousands of patients in a reasonable time frame remains a challenge, Lei said.
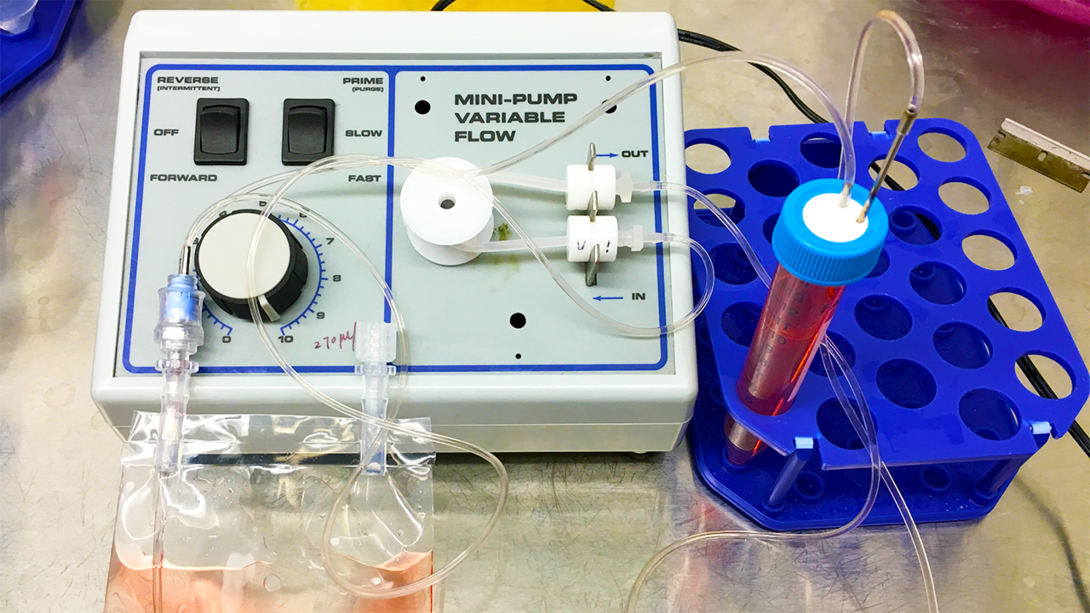
The researchers demonstrated that, given about a week and less than a teaspoon of hydrogel, its prototype could grow and differentiate 1 million induced pluripotent stem cells into roughly 50 million neural stem cells. They also calculated that tripling the size of the tube and culturing with eight teaspoons of hydrogel would allow them to grow about 1 billion cells in the same span.
A month after researchers transplanted the resulting neural cells into the brains of rats, they found that substantial numbers of cells had survived and developed into human neurons. Lei said the results, which the team reported in the journal Scientific Reports, bode well for hydrogel culturing systems, even as he acknowledged that much work remains before taking such technology from the bench to the bedside.
“Manufacturing therapeutic cells is still at a very early stage of development,” said Lei, who has a patent pending via NUtech Ventures. “We really need a lot of innovation in cell-manufacturing technology.
“But if you have an affordable and highly efficient culture system, you can do a lot of good.”
Lei authored the study with Haishuang Lin, postdoctoral researcher in chemical and biomolecular engineering, and Qiang Li, graduate student in chemical and biomolecular engineering. The team received support from the Nebraska Department of Health and Human Services.