
As hosting gigs go, it’s a tough crowd.
More than 1 billion people are host to parasitic worms that take up residence in their intestines. For most, it’s a short stay, with the immune system evicting the worms in days or weeks and leaving no trace that the parasites were ever there.
In a small percentage of people and other animals, though, the worms gain a permanent mouth-hold and can stick around the intestines for years. That persistence often leads to malnutrition, which in turn tightens the grip of infection, initiating a spiral that becomes difficult to escape.
The question of why that small percentage struggles to expel parasites has stymied researchers for a while. But a new mathematical model developed at the University of Nebraska-Lincoln and Royal Netherlands Institute for Sea Research offers an answer while reinforcing an adage: safety in numbers.
Clay Cressler, Anieke van Leeuwen and their colleagues have concluded that when large numbers of worms stake out intestinal territory in a host, they generally manage to hang in there for the long term. By contrast, the model suggests that lone worms — or small groups of them — get overwhelmed by the immune system and quickly flushed from the GI tract.
“Some hosts get sick for a really long time. Some clear (parasites) really fast,” said Cressler, assistant professor of biological sciences at Nebraska. “That’s not something that could be explained with the theory we had before.”

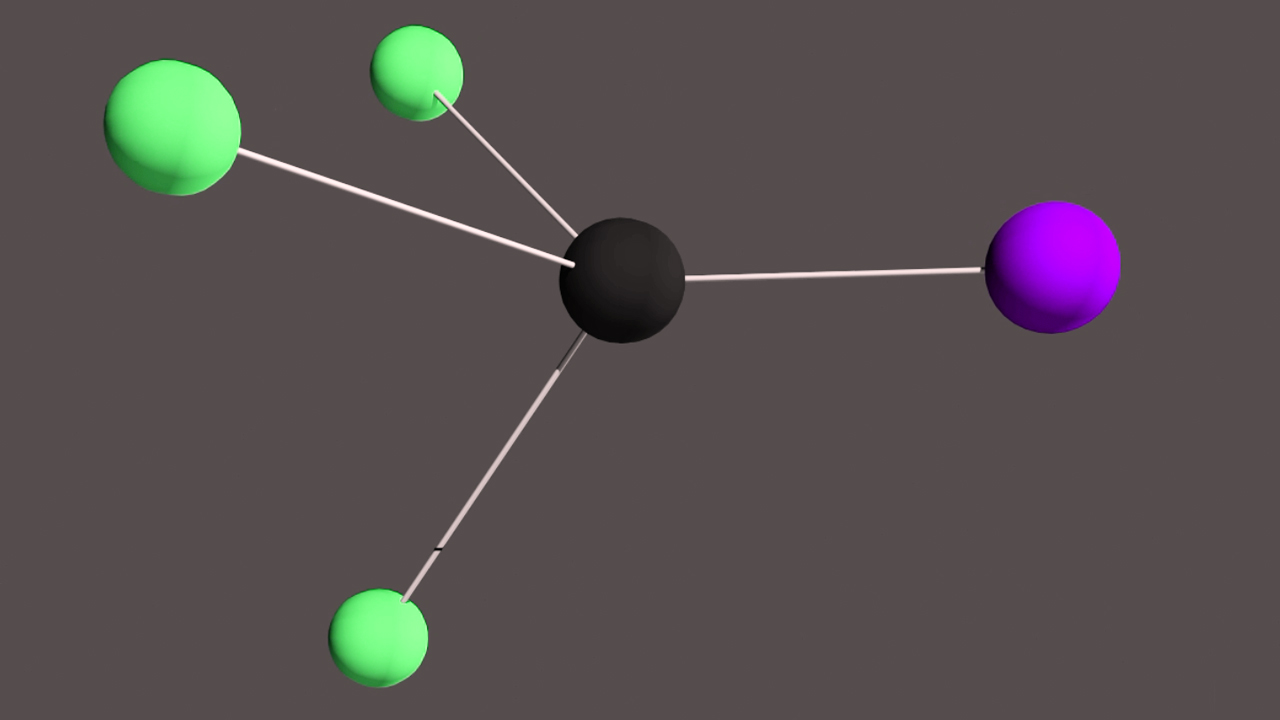
The team’s model can simulate host-parasite interactions by accounting for multiple variables: number of parasites, availability of food, body mass of the host, how much of that mass is accessible to parasites vs. the immune system. Crucially, it also factors in that parasitic worms can manipulate a host’s ability to digest food and mount an immune response.
As part of a recent study, the team simulated whipworm infections for 1,000 mice while varying the number of worms that infected their colons. From those results, the researchers deduced that a large collective of whipworms can kick-start a self-perpetuating cycle that nearly guarantees the parasites’ survival.
Though the specifics aren’t totally clear, prior research has led the team to suspect that a critical mass of worms may unleash a barrage of molecules that confuse or suppress the immune system and allow the parasites to begin high-jacking a host’s nutrients.
“Anything that a parasite does to increase its own access to resources indirectly deprives the host of them,” Cressler said. “The more parasites there are, the better they are at manipulating resources, and the better they are at manipulating, the better the parasites grow. And then they’re even better at manipulating. So you get this positive-feedback loop that allows them to establish a chronic infection.”

When a moderate number of worms infect a host, their length of stay becomes less certain and seems to depend more on other factors: How large are the host’s fat reserves? Has its immune system already been primed to respond? How much is it eating?
On the latter question, the team found evidence that more food increases the odds of a long-term stay.
“Historically, the perspective is that food really only matters for the host,” Cressler said. “Only recently, within the last 10 years or so, has there been more of a focus on what diet is doing to the parasite. Is there a chance that what you’re actually doing is just feeding the parasite more? In this case, that’s what happens.
“If (biological) systems are frequently in this place where you can go either way, then small changes in other things that we’re not (historically) paying attention to can be the things that determine whether you go one way or the other.”
Yet when all other factors are equal, the model indicates that the quantity of parasitic worms alone may determine whether they persist in a host. That’s a potentially important advance, Cressler said, given that prior approaches have mostly treated parasite duration as a fixed, independent variable rather than one dependent on other factors.
And when the team compiled the fates of each mouse in its simulation, the resulting distribution resembled the pattern commonly seen in nature: most hosts burdened with just a few parasites, a few hosts burdened with many.
“Most of the theory that we use in understanding immune-parasite interactions is insufficient to address the question of where this kind of variation comes from,” Cressler said. “If you have this ability to (allow for) either long duration or short duration, what you end up seeing are many hosts who keep getting the short-term infections and have very low burdens, and some hosts who will keep getting these long-term infections and end up with a very high burden.
“So this hypothesis could potentially help to explain two big patterns in parasitology: this widespread variation in how long infections last and this widespread variation in how sick each host is.”
Though the team’s model first needs to withstand the scrutiny of experimentation and further research, Cressler said, it might eventually help inform the treatment of parasitic infections or calibrate predictions of chronic cases. Doing so before potentially chronic infections result in malnutrition — and diminish the usefulness of drugs that otherwise clear parasites — could prove especially valuable in the developing world.
“If we could (eventually) tell you, ‘This is the stuff you need to measure to know whether somebody is going to be chronically infected,’ then that might tell you something about how you need to treat or who you need to treat,” Cressler said. “Where’s the highest-risk area, where the environment is such that people are going to be primed toward this chronic rather than acute infection?
“This variation in duration is a real pattern, and it has real consequences for people. Anything we can do that helps to understand how these infections work could potentially have a therapeutic value later. We don’t know what that is now. But that’s the goal.”
The researchers reported their findings in the journal Proceedings of the Royal Society B. Cressler and van Leeuwen authored the study with Andrea Graham of Princeton University and Sarah Budischak of Claremont McKenna, Pitzer and Scripps Colleges. The team received support from the National Science Foundation.
Share
News Release Contact(s)
Related Links
Tags
High Resolution Photos
HIGH RESOLUTION PHOTOS








