A University of Nebraska–Lincoln researcher is leading a team using National Institutes of Health funding to investigate how interpersonal discrimination gets “under the skin” for Latinos, creating wear and tear on the body that may ultimately lead to chronic health conditions like cardiovascular disease.
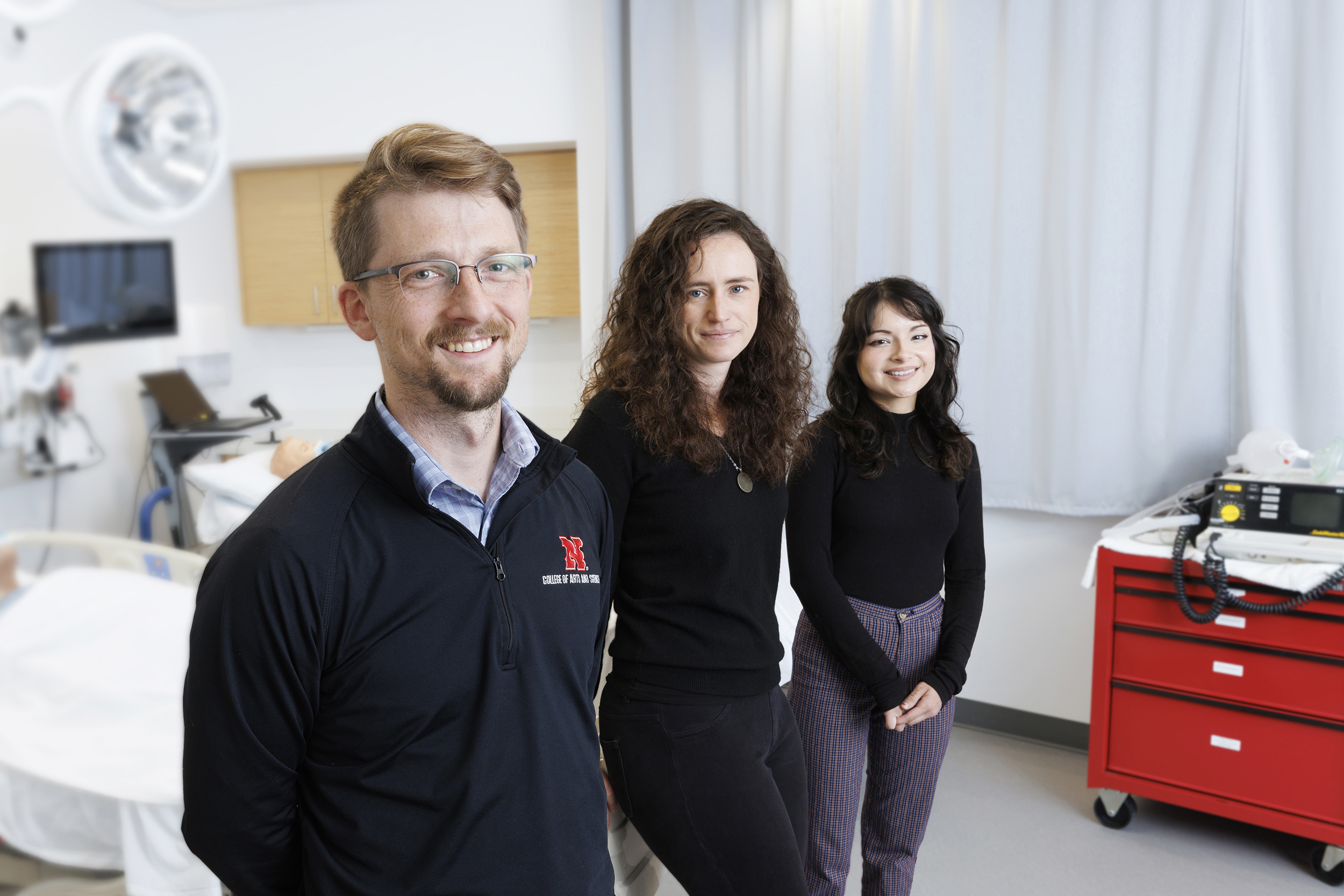
Nebraska psychologist Arthur “Trey” Andrews recently received a four-year, $2.5 million NIH grant for a project that will reframe the role of interpersonal discrimination in driving chronic stress and health inequities among Hispanics. Rather than studying how episodes of discrimination affect people on an individual level — the traditional approach — Andrews’ approach recognizes that stress stemming from discrimination may ripple across a social network, impacting its collective health.
But social networks are also key to resilience: Numerous studies show that supportive social ties blunt the effects of stress and reduce inflammatory biomarkers that predict long-term physical health. Andrews hopes to apply this concept to discrimination-induced stress by pinpointing how social networks can confer health resilience against discrimination — while avoiding the spillover stress that can spread when people are in vulnerable positions without the support they need.
“We’re really getting at this notion about how discrimination stress, and really stress in general, doesn’t stay within the individual,” said Andrews, associate professor of psychology and ethnic studies and associate director of the university’s Minority Health Disparities Initiative. “We aren’t isolated islands. Those around us help us carry that stress. This is really about trying to understand when and how does that happen, and when and how are those around us more helpful in really easing the stress and burden that comes along with experiencing discrimination.”
The team will first determine how exposure to discrimination affects a person’s allostatic load, or the bodily wear and tear from stress. Allostatic load likely underlies the Weathering Hypothesis, which suggests that exposure to social and economic disadvantage, including interpersonal discrimination, accelerates poor health outcomes across a wide range of conditions.
Prior research on discrimination-related stress has measured it via self-report. Andrews’ approach instead adopts a standardized assessment of discrimination stress that uses noninvasive physiological biomarkers and stress reactivity tests. The team will connect these results to standard markers of allostatic load to understand how stress responses relate to the wear and tear that builds up over time.
Andrews’ team will periodically measure participants’ cholesterol, an inflammation-related protein, a diabetes indicator and more — all markers of stress-related breakdown in the body among Hispanics living in the United States.
Andrews is predicting that allostatic load will increase in people who have a strong physical reaction to discrimination stress and who frequently experience such stress.
The team will then study discrimination and its health effects in the context of a social network. The roughly 400 Hispanic people participating in the project will be recruited via respondent-driven sampling, whereby participants invite their social contacts to join the study, guaranteeing the population sample represents a social network.
Sara Reyes, community coordinator for the Minority Health Disparities Initiative, will serve as the project coordinator. Reyes, a Latina from Nebraska who is fluent in Spanish and English, will build on the initial 100-member cohort she’s already recruited. She will also oversee day-to-day project activities, data collection and communication with participants, using their feedback to guide the project’s trajectory.
When recruitment is complete, Andrews’ team will use Open Dynamic Interaction Network, a software platform developed by project co-investigator and former Husker researcher Bilal Khan. The system will prompt participants to answer questions about the discrimination they experienced each day and the related social support they received or gave. Those questions could be supplemented by the system’s use of Bluetooth data from participants’ cellphones to anonymously detect when participants are in close proximity to each other.
Andrews and the team will use those data and advanced modeling techniques to paint a clearer picture of how discrimination stress cascades across a network and illuminate the network characteristics that mitigate stress. The analysis will provide important clues about how real-world practices and policies can curb the chronic stress of repeatedly encountering discrimination.
For example, Andrews said the study results may help institutions and workplaces launch successful mentorship or support programs that help people who face discrimination. Currently, organizations often appoint just one person to serve as a mentor. But if that person doesn’t have a strong support network of their own, serving in the role may be detrimental from a mental health standpoint.
“We hope our results may speak to when this type of setup is a risky venture and may be more harmful, and when it could be beneficial,” Andrews said. “We need to really consider how effective support can really happen.”
Andrews said the findings could also help institutions implement effective hiring and retention practices, and guide clinical providers as they make recommendations for people seeking social support.
Co-investigators include Reyes; Husker faculty Timothy Nelson, Tierney Lorenz and Patrick Habecker; and Khan, now at Lehigh University.