Cellular metabolism is emerging as a critical factor in controlling the immune system’s response to pathogens that cause human disease, as well as the activity of cancerous cells. A University of Nebraska–Lincoln scientist is studying how those relationships evolve, with an eye toward development of therapeutics or drugs that could give the immune system an edge over these sometimes deadly enemies.
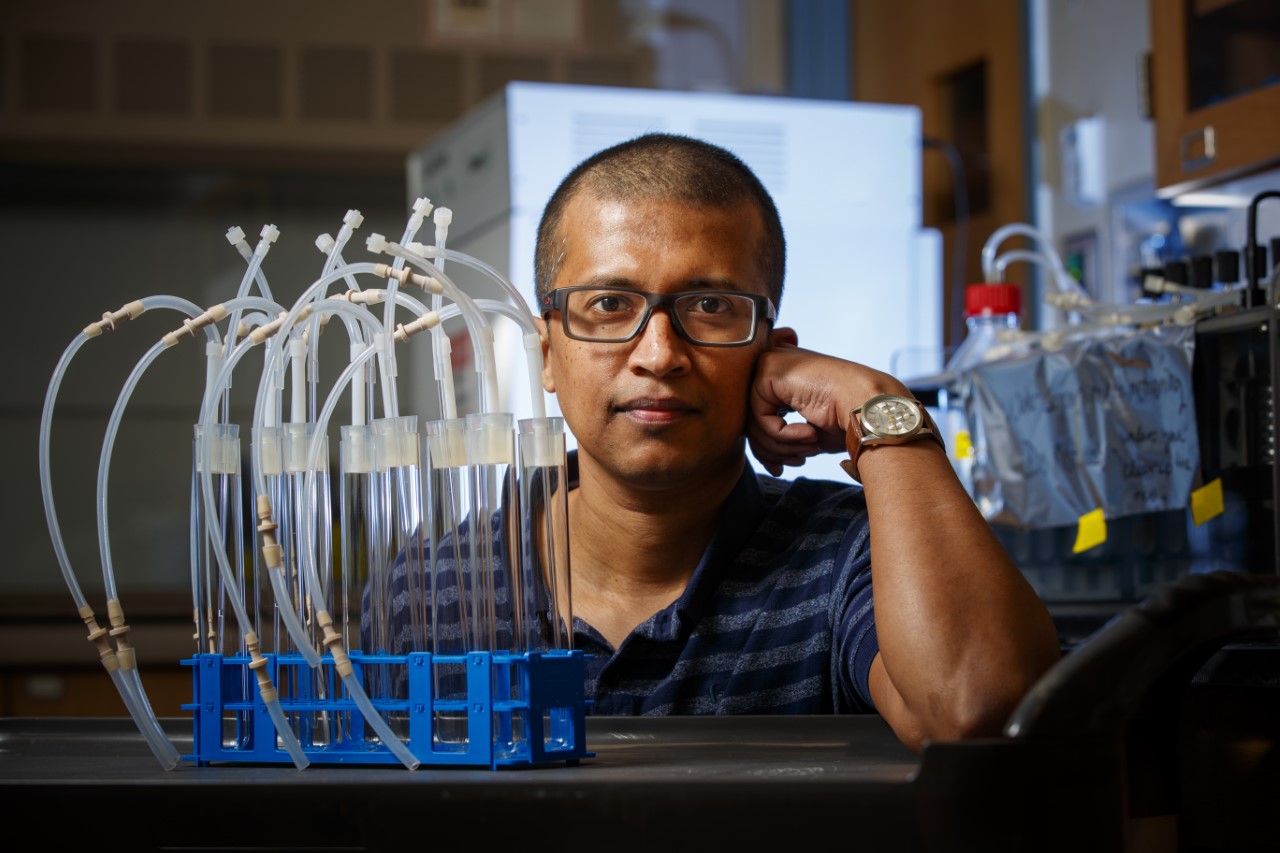
“We would like to know how our white blood cells interact with infections … both pathogenic infections from a bacteria or viral strain … and also nonpathogenic infections such as cancer,” said Rajib Saha, assistant professor of chemical and biomolecular engineering.
Saha has received a five-year, $1.8 million Maximizing Investigators Research Award from the U.S. Department of Health and Human Services to support his research.
Saha’s work will focus on the dynamic metabolic shifts in specific types of white blood cells such as macrophages; lymphocytes; and mast cells upon infections caused by pathogens Staphylococcus aureus, a bacterium that is linked to as many as 50,000 deaths a year in the U.S., and SARS-CoV-2, the virus that causes COVID-19. His team also will study these immune cells’ impact on pancreatic cancer’s cell metabolism and if cellular changes affect severity of the disease.
White blood cells are resilient and flexible, critical to their role in fighting disease, Saha said. His research aims to learn what key changes occur between those cells and the diseases they’re fighting so scientists can develop approaches to boost the immune system in those battles.
“We’d like to know how white blood cells interact in these different scenarios and what kind of changes happen in the white blood cells’ metabolism so that we can learn and develop therapeutics in the future,” Saha said.
“To do that, we need to define, ‘These are the key fingerprints for a healthy cell. And these are the key fingerprints for a diseased cell.’”
Scientists already believe white blood cells’ metabolism plays a critical role in dictating the severity of pathogenic infection — whether asymptomatic, mild or severe — and in controlling both genetic and epigenetic phenomena in a cancer cell. But to what extent changes in the host’s immune system affect that role is still unclear.
Saha’s work is computational, not lab-based. His team uses existing data in creating computer models for both white blood cells and pathogens. The models then interact with each other to determine how cells and pathogens might interact in a host. Later, colleagues will test Saha’s findings in the lab to validate or discount them.
Saha’s research will build on his team’s earlier success in developing a predictive and accurate modeling framework to track the time-dependent changes of cellular metabolism.
Ultimately, his findings could provide scientists including molecular biologists, computational biologists, clinicians and translational scientists with a basic understanding of metabolism’s role in dictating disease severity and also a useful template to investigate other diseases.
Saha’s collaborators include colleagues from the University of Nebraska Medical Center.