Every 40 seconds, somewhere in the United States, a person suffers a stroke. Early treatment is important in stopping further damage to the brain, and a University of Nebraska-Lincoln researcher is working to revolutionize front-line stroke care.
Husker scientist Steven Barlow and Hyuntaek Oh, who earned his doctorate from Nebraska, have published the first in a series of studies that show the effectiveness of a device known as the Galileo TAC-Cell Array as a potential emergency-room treatment for embolic stroke sufferers.
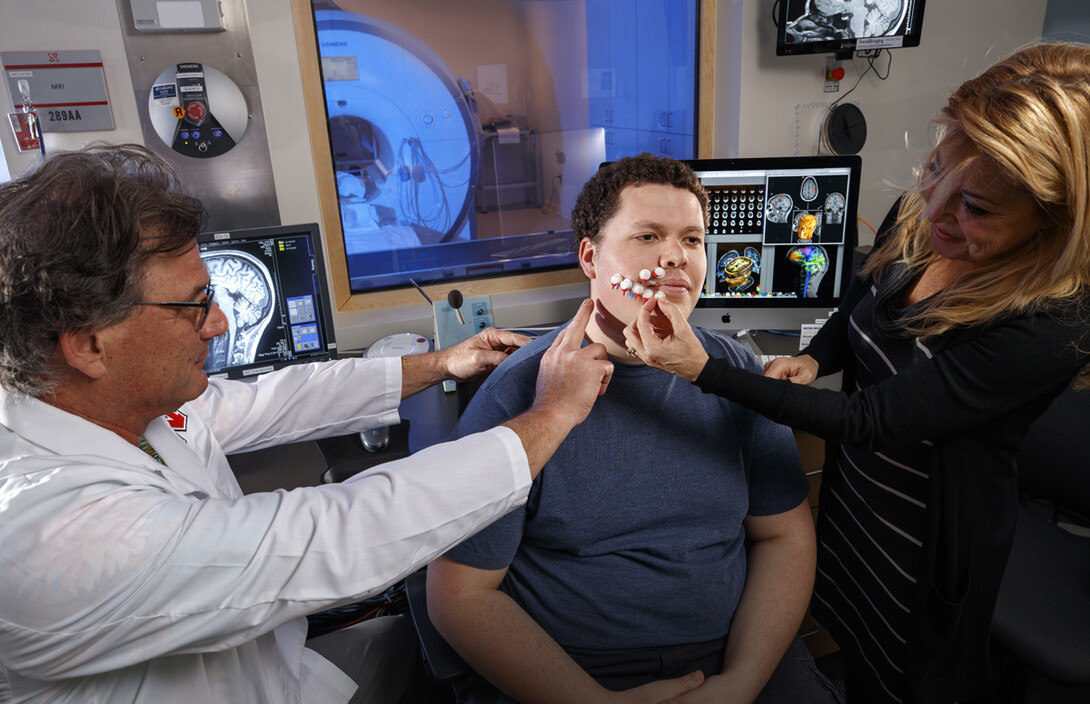
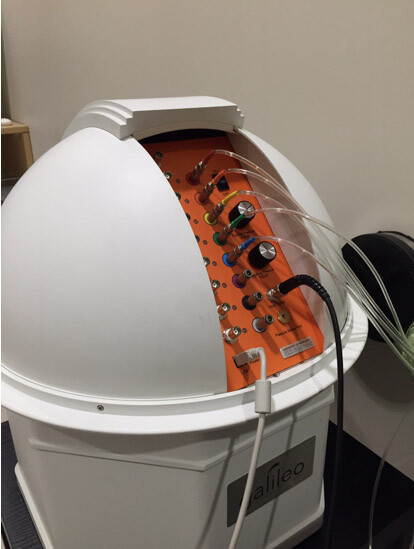
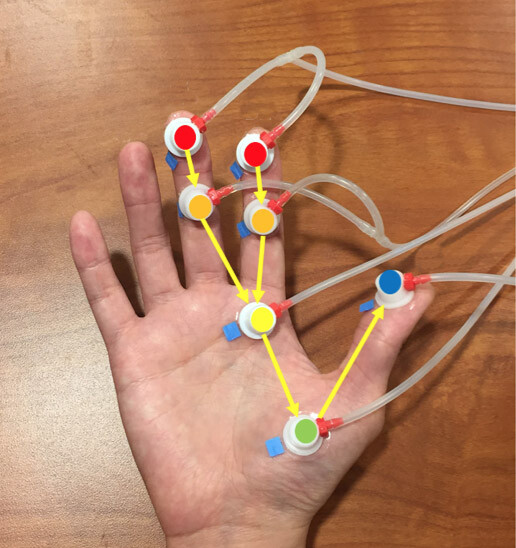
Galileo utilizes pressurized air as a non-invasive method of brain stimulation. The 19-inch-tall, domed machine produces air pulses at supersonic speeds that are sent through small plastic tubes into capsules that are applied to the hands or face to create a nerve response.
The study, published Aug. 25 in the journal PLOS One and co-authored by Oh, Barlow, and fellow scientists Rebecca Custead and Yingying Wang, is also the first that was designed and conducted using the functional Magnetic Resonance Imaging technology in the university’s state-of-the-art Center for Brain, Biology and Behavior, where one of the core missions is to improve treatment for traumatic brain injury.
Transforming treatment could save lives, and billions of dollars. Embolic stroke – the cutoff of blood flow to an area of the brain, usually caused by a blood clot – is the fifth-leading cause of death in the United States, according to the Centers for Disease Control and Prevention. It also is a leading cause of long-term disability because patients lose mobility following brain and nerve cell death.
Galileo, invented by Barlow as a brain research tool when he was at the University of Kansas, is applied to the skin in specific patterns and speeds to activate the brain’s cerebral cortex and cerebellum and increase blood flow. After seeing the research performed with Galileo, Barlow suspected it could be a novel treatment for stroke. Animal studies performed at other institutions showed tactile, or touch, stimulation with features similar to Galileo re-routes blood flow to areas of the brain where the main blood source has been cut off, preventing damage to brain cells, if applied within two hours of blood cutoff.
If the machine were used in emergency rooms, Barlow said, it could non-invasively reverse the effects of a stroke.
“It’s a natural form of stimulation, so our patterned somatosensory stimulation recruits and activates nerve cells in the appropriate order, whereas other modalities, like electrical stimulation may activate neurons in atypical order,” Barlow, Corwin Moore Professor of special education and communication disorders and assistant director of CB3, said. “Because it is non-invasive, we can use this in infants, children, in all sorts of neurologic populations.”
Barlow’s study establishes best practices for treatment in stroke victims by examining effects of Galileo stimulation in healthy adults. The initial study included experiments performed on the hand. A study regarding stimulation to the face is forthcoming, Barlow said.
By using fMRI technology in CB3, Barlow’s research team determined the optimal speeds and patterns of tactile stimuli that provided the best blood-oxygen level dependent response in the brain. The greatest response was elicited from stimulation traveling up the hand at 25 centimeters per second.
As he awaits publication of additional Galileo research, he is readying a funding application for the National Institutes of Health to partner with the University of Nebraska Medical Center’s Nebraska Stroke Center, which will bring the therapy to Nebraska Medicine, and is a crucial step in gaining approval from the Federal Drug Administration.
“It’s an example of bench-to-bedside research,” Barlow said. “We have to come up with the data in a clinical population to demonstrate efficacy for FDA.”
Barlow also hopes to redesign the Galileo to make it smaller, possibly the size of an old-fashioned black lunch pail, so that it could be used in ambulances and start therapy at the scene.
“That’s the view with binoculars,” he said.
Barlow said the CB3’s dedication to research will help him and his laboratory team bring neurotherapeutic applications using Galileo technology to market faster.
“This is extremely rare to have a research-dedicated neuroimaging center at the university that is not obliged to run clinical scans in a medical school setting,” Barlow said.







