· 3 min read
Normal blood flow may stabilize plaque, lower odds of cardiac events

Welcome to Pocket Science: a glimpse at recent research from Husker scientists and engineers. For those who want to quickly learn the “What,” “So what” and “Now what” of Husker research.
What?
Plaque afflicts more than just teeth. A cholesterol-infused version of the stuff can also coat the inner lining of arteries, sometimes hardening and narrowing those canals to the point that oxygen-ferrying blood slows and struggles to reach the heart. Yet the rupturing of those fatty plaques can prove even more dangerous, causing blood clots that block arteries, yielding heart attacks and strokes.
Though high cholesterol affects all arteries the same, plaques usually form around curves and forks that tend to disturb blood flow. Arterial straightaways, by contrast, enjoy normal blood flow that helps protect against plaque formation. But less is known about how, if at all, normal blood flow may modify plaque that has already rooted itself to arterial walls.
So what?
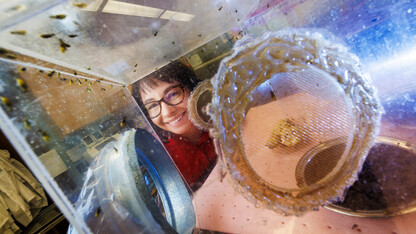
Nebraska’s Ryan Pedrigi, Morgan Schake, Ian McCue and colleagues decided to test a hypothesis: that blood flowing at typical speed stabilizes existing plaque, lowering the odds of it breaking free and kick-starting acute trauma.
The team’s experiment involved cuffing the carotid arteries of mice for multiple weeks, long enough to induce a moderate buildup of plaque. The researchers then evaluated three treatments: retaining the cuffs but introducing daily doses of atorvastatin (Lipitor), a medication that lowers blood cholesterol; removing the cuffs to restore normal blood flow; or both.
As expected, atorvastatin by itself showed signs of stabilizing plaques when compared against untreated mice. But mice that lost the cuffs without receiving the meds showed similar improvement. Compared with their cuff-wearing counterparts, the mice saw a 72% drop in lipids and macrophages — both markers of plaque instability and progression — and an 89% jump in collagen, a marker of stability, in plaques otherwise prone to destabilization.
The fact that simply restoring normal blood flow could mimic the beneficial effects of atorvastatin is “remarkable,” the researchers said, given that the latter can reduce the 10-year incidence of heart attack by up to 23%. The combination of atorvastatin and decuffing, meanwhile, appeared to not only stabilize the plaques, but notably reduce their size.
Now what?
Learning why normal blood flow is therapeutic, and how to artificially recreate its effects, rank at the top of the to-do list. Ultimately, the study could inform the development of a non-invasive therapeutic that can target diseased arteries, the team said, and be paired with cholesterol-lowering meds to combat the life-threatening consequences of plaque buildup.